The Nipah virus (NiV) is a zoonotic virus which means it can be transmitted from animals to humans. It belongs to the family of paramyxoviruses. Humans can contract this virus through direct contact with infected animals, like bats, and pigs or it can spread through contaminated food. It can also spread from person to person. It shows symptoms like common fever and problems related to respiration. It is a cause of concern due to multiple outbreaks in the recent past, particularly in South and Southeast Asia. Presently there is no vaccine available for the virus.
Origin of Nipah Virus
The Nipah Virus first appeared in Malaysian pig farmers in 1999. In 2001, it was detected in Bangladesh, and at the same time, it was also found in eastern India.
- Global spread: The traces of the virus have been identified in Cambodia, Ghana, and Thailand.
- Nipah’s contact with India: In India, the first Nipah virus outbreak occurred in Siliguri, West Bengal, in the year 2001. The outbreak again happened in the year 2007.
- The 2001 outbreak indicated possible human-to-human transmission, with health workers in Siliguri getting infected.
- Recently, Kerala also experienced a Nipah outbreak.
Structure of Nipah Virus
NiV is a single-stranded, enclosed, negative-sense RNAvirus. It is a member of the Henipavirus genus, which is part of the Paramyxoviridae family. The NiV‘s structure is defined by many main components:
- NiV’s nucleocapsid is protected by a matrix protein, which contains prominent fusion proteins and glycoproteins required for attachment and entry into cells.
- It shows a distinct cytoplasmic structure close to the endoplasmic reticulum.
- Genome structure: The NiV genome is a negative-sense single-stranded RNA. It generates structural proteins like N, P, M, F, G, and L.

Nipah Virus Transmission
The ability of the Nipah virus to spread in multiple ways makes it difficult for public health personnel to detect the virus. Some of the ways in which the virus can be transmitted are:
- Direct contact: The infection can occur through direct contact with infected animals, such as bats or pigs, particularly through their bodily fluids.
- Consumption of contaminated food: In Bangladesh and India, the main source of the Nipah virus is eating fruits, which are contaminated with the saliva of infected fruit bats.
- Testing:
- Real-time polymerase chain reaction (RT-PCR), Immunohistochemistry (IHC), Enzyme-linked immunosorbent assay (ELISA) and Serum neutralisation test (SNT) are some tests available to detect the virus.

Nipah Virus Symptoms
The virus shows respiratory and neurological issues. It is easily transmissible. It can spread from infected animals and individuals. This dual mode of transmission makes it a major cause of concern.
- Common signs: The infected person shows fever, head pain, muscle aches, nausea, and a scratchy throat.
- Progression: It shows symptoms such as dizziness, drowsiness, and neurological signs suggestive of acute encephalitis may appear.
- Severe cases: The seizures can occur in severe cases, leading to a coma within 24 to 48 hours.
- Severity: It can cause mild to severe disease, including swelling of the brain (encephalitis) and potentially death.

Treatment of Nipah Virus
There is currently no known treatment or vaccine available for humans or animals.
- However, Ribavirin, an antiviral, may play a role in lowering mortality in patients with Nipah virus encephalitis.
- The main approach to managing the infection in people is intensive supportive care combined with symptom treatment.
Current Trends
Current Nipah virus trends indicate that outbreaks are frequently seasonal and region-specific. Concerns have recently centred on the possibility of increased human-to-human transmission, which could make the virus more contagious. Kerala has seen several outbreaks in the last five years, the most recent in 2023.
- Transmission pattern evolution: While the first outbreaks involved bats to pigs and then pigs to humans, later outbreaks, particularly in India, demonstrated direct bat-to-human and human-to-human transmission.
- Regular outbreaks: From 2001 to 2015, Bangladesh experienced frequent NiV outbreaks. In the 2018 outbreak in Kerala around 17 people were killed. In September 2023 Kerala reported sex confirmed cases, including two deaths.
India’s strategy for Nipah Virus Outbreak
India responded with the following measures to contain the Nipah virus outbreak in Kerala.
- Coordination: Kerala’s Health Department mobilised multiple teams for containment and mitigation of the virus with the support of the Indian government. They formed 19 core committees to oversee various response measures.
- Surveillance: Over 53,000 houses were surveyed during active house-to-house surveillance in containment zones.
- Movement restrictions: A total of nine villages in Kozhikode had movement restrictions, mandatory mask-wearing, and social distancing.
- Laboratory testing: Multiple labs conducted tests on suspected cases and environmental samples.
- Health facility preparedness: Emergency rooms were prepared to handle cases. Isolation rooms, ICU beds, and ventilators had all been prepared.
- Public awareness: It was raised through press releases, expert videos, and a call centre. Anti-fake news measures have been implemented.
- Guidelines: The response measures were developed with WHO assistance during the 2018 Nipah outbreak in Kerala.
Comprehensive Prevention Strategies
In areas where Nipah virus (NiV) outbreaks have occurred, quarantine measures should be followed to prevent the further transmission of the virus. The hospital in the area should follow standard infection control practices to stop the spread of the virus within the hospital community.
- Exploring new methods: Invest in new technologies or techniques to curtail the spread of the virus among bat populations, like the use of drones for surveillance.
- Prompt detection: Develop and improve tools to detect the virus early in communities and livestock.
- Healthcare: Follow the strict guidelines in healthcare environments to prevent the virus from spreading from person to person.
- Public awareness: Educate the populations that are at higher risk and show the signs, symptoms, and risks associated with NiV.
- Flying fox habitats: NiV outbreaks are more likely in areas with flying fox habitats (genus Pteropus). Residents and visitors to these areas should take precautions similar to those taken in areas with known NiV incidents.
Last updated on July, 2025
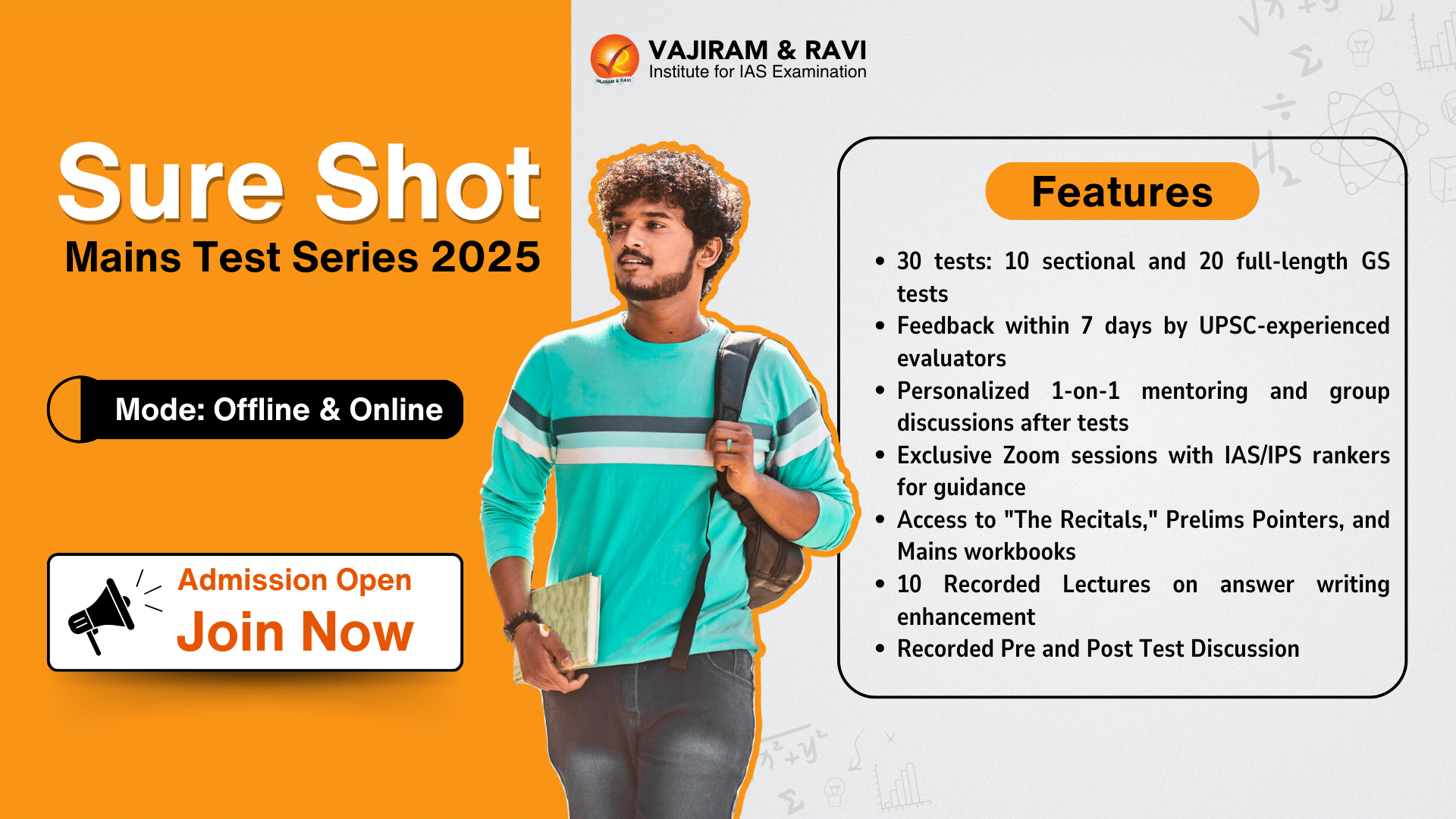
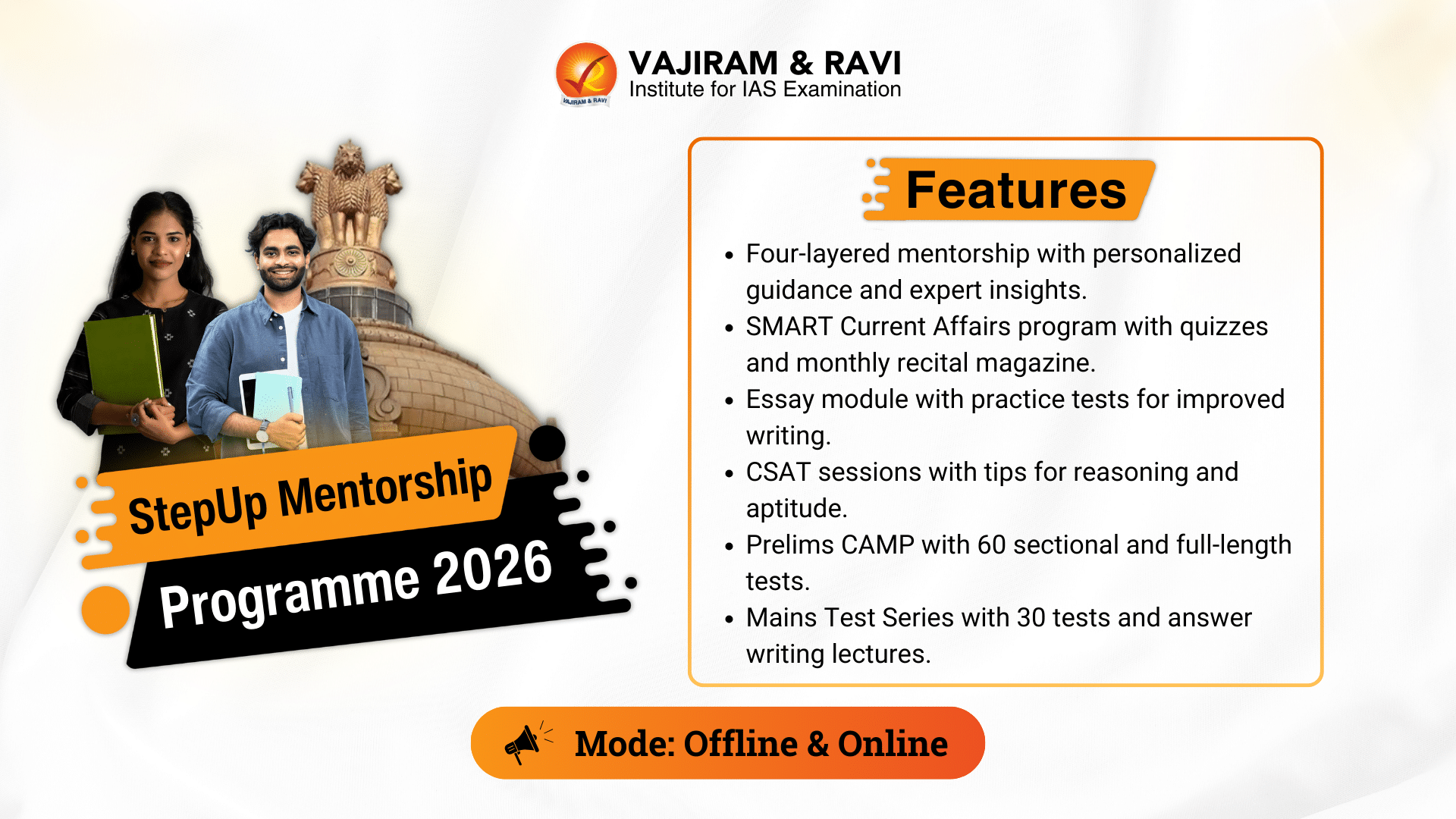
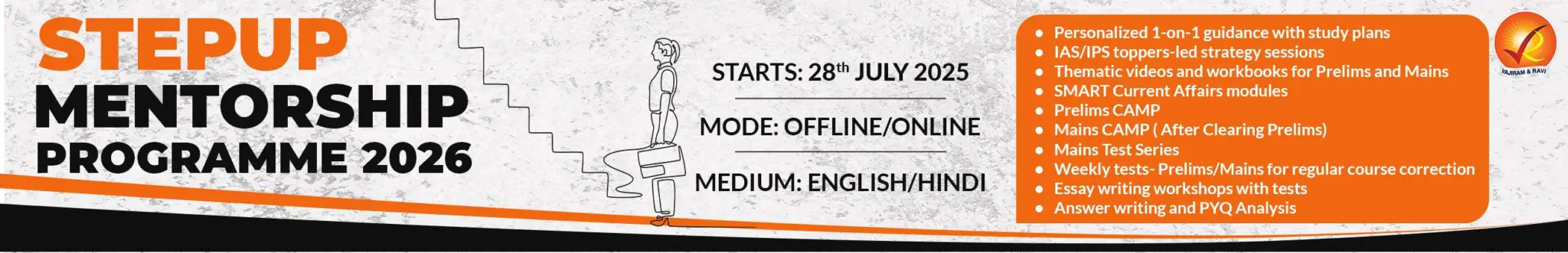
→ UPSC Notification 2025 was released on 22nd January 2025.
→ UPSC Prelims Result 2025 is out now for the CSE held on 25 May 2025.
→ UPSC Prelims Question Paper 2025 and Unofficial Prelims Answer Key 2025 are available now.
→ UPSC Calendar 2026 is released on 15th May, 2025.
→ The UPSC Vacancy 2025 were released 1129, out of which 979 were for UPSC CSE and remaining 150 are for UPSC IFoS.
→ UPSC Mains 2025 will be conducted on 22nd August 2025.
→ UPSC Prelims 2026 will be conducted on 24th May, 2026 & UPSC Mains 2026 will be conducted on 21st August 2026.
→ The UPSC Selection Process is of 3 stages-Prelims, Mains and Interview.
→ UPSC Result 2024 is released with latest UPSC Marksheet 2024. Check Now!
→ UPSC Toppers List 2024 is released now. Shakti Dubey is UPSC AIR 1 2024 Topper.
→ Also check Best IAS Coaching in Delhi
Tags: nipah virus quest