What’s in today’s article?
- Why in News?
- What was the Background in which the MHA was Enacted?
- What Does the Mental Healthcare Act 2017 Say?
- What are the Challenges to Implementation of MHA?
- What Needs to be Done to Strengthen Mental Healthcare?
Why in News?
- The National Human Rights Commission (NHRC) in a report flagged the “inhuman and deplorable” condition of all 46 government-run mental healthcare institutions across the country.
- The NHRC’s observations were made after visits to all operational government facilities, to assess the implementation of the Mental Healthcare Act (MHA), 2017.
What was the Background in which the MHA was Enacted?
- MHA’s predecessor – the Mental Healthcare Act, 1987, prioritised the institutionalisation of mentally-ill people and did not afford any rights to the patient.
- It also provided disproportionate authority to judicial officers and mental health establishments to authorise long-stay admissions against the informed consent of the individual.
- The 1987 Act embodied the ethos of the colonial-era Indian Lunacy Act, 1912, which linked criminality and madness.
- Hence, the intention was never to define illness but to protect social order, which –
- Not only violates Article 21 of the Indian Constitution which protects personal liberty,
- But it also indicates a failure of the government(s) to discharge the obligation under various UN Conventions (ratified by India) relating to rights of persons with disabilities.
- The MHA 2017 was a watershed moment for the right to health movement in India, after the enactment of the Rights of Persons with Disabilities Act of 2016.
- This was the first time a psychosocial approach (not only a psychiatric approach) to mental healthcare was adopted and has shifted from providing only treatment to centring the rights and the will of the person.
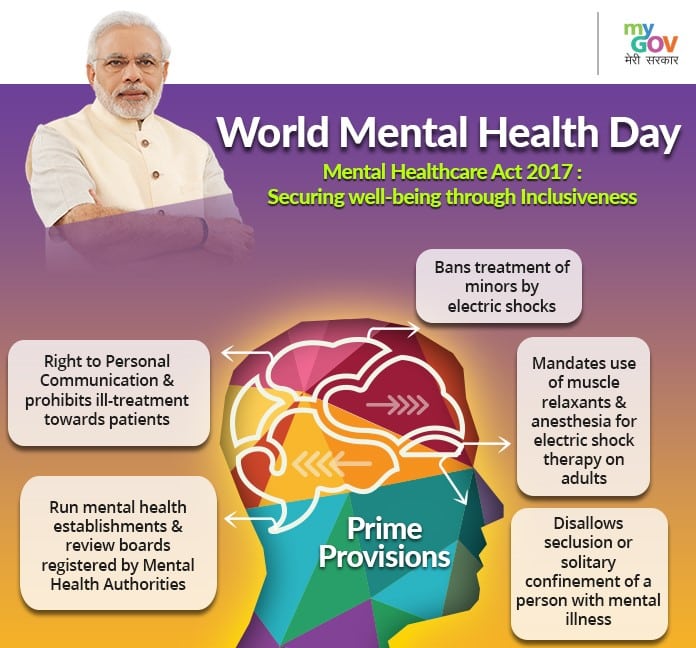
What Does the Mental Healthcare Act 2017 Say?
- It discourages long-term institutionalisation of patients and reaffirms the rights of people to live independently and within communities.
- The government was made responsible for creating opportunities to access less restrictive options for community living – such as halfway homes, rehab homes, etc.
- The Act also discourages using physical restraints (such as chaining), objects to unmodified electro-convulsive therapy (ECT).
- It pushes for the rights to hygiene, sanitation, food, recreation, privacy, and infrastructure and recognises that people have a capacity of their own (unless proven otherwise).
- It also empowers people to make “advance directives” and can nominate a representative for themselves.
What are the Challenges to Implementation of MHA?
- According to a 2018 report, almost 36.25% of residential service users at state psychiatric facilities were found to be living for one year or more in these facilities.
- The main reasons are –
- Non-compliance to MHA regulations,
- Absence of community-based services, and
- Social stigma that looks at a person with mental illness as a “criminal” deserving of incarceration.
- Under the MHA, all States are required to establish a State Mental Health Authority and Mental Health Review Boards (MHRBs), to oversee the functioning of the mental healthcare institutes.
- In a majority of the States, these bodies are yet to be established or remain defunct, which makes redressal in case of rights violations difficult.
- In 2022, the Bombay HC held that mental healthcare institutes do not routinely assess the condition of patients to ascertain if they can be discharged.
- Poor budgetary allocation and utilisation of funds further create a scenario where shelter homes remain underequipped, understaffed, service providers are not adequately trained, etc.
- People are either put in these establishments by families or through the police and judiciary. In many cases, families refuse to take them because of the social stigma.
- Gender discrimination plays a role here, as women are more likely to be abandoned due to family disruption, marital discords and violence in intimate relationships.
- The dearth of alternative community-based services and socio-economic opportunities further complicates access to rehabilitation.
What Needs to be Done to Strengthen Mental Healthcare?
- The State Mental Health Authority should meet at least four times (as mandated under the Act), to oversee that the entire mental healthcare system is functioning effectively.
- The model of reintegration and recovery (needs to be replicated elsewhere):
- Chennai’s Institute of Mental Health launched five halfway homes, where people can access the confidence and skills needed to manage themselves outside a structured institution.
- Kerala has also started half-way homes and community living centres, providing rehabilitation to people who are abandoned by family members.
- The need of the hour is to implement rights and recovery-based approaches to change attitudes and practices on the ground.
Q1) How the Mental Health Act 2017 evolved?
The Mental Healthcare Act 1987 embodied the ethos of the colonial-era Indian Lunacy Act, 1912, which linked criminality and madness. Hence the 2017 Act was a watershed moment for the right to health movement in India. This was the first time a psychosocial approach to mental healthcare was adopted.
Q2) What are the salient provisions of the Mental Health Act 2017?
It discourages long-term institutionalisation of patients. The government was made responsible for creating opportunities to access less restrictive options for community living. The Act also discourages using physical restraints, pushes for the rights to hygiene, and empowers people to make “advance directives.”
Source: Does India’s Mental Healthcare Act, 2017 protect patients’ rights and dignity in institutions?
VIDEO: https://www.youtube.com/watch?v=FAiCv_zRMtw
Last updated on June, 2025
→ UPSC Notification 2025 was released on 22nd January 2025.
→ UPSC Prelims Result 2025 is out now for the CSE held on 25 May 2025.
→ UPSC Prelims Question Paper 2025 and Unofficial Prelims Answer Key 2025 are available now.
→ UPSC Calendar 2026 is released on 15th May, 2025.
→ The UPSC Vacancy 2025 were released 1129, out of which 979 were for UPSC CSE and remaining 150 are for UPSC IFoS.
→ UPSC Mains 2025 will be conducted on 22nd August 2025.
→ UPSC Prelims 2026 will be conducted on 24th May, 2026 & UPSC Mains 2026 will be conducted on 21st August 2026.
→ The UPSC Selection Process is of 3 stages-Prelims, Mains and Interview.
→ UPSC Result 2024 is released with latest UPSC Marksheet 2024. Check Now!
→ UPSC Toppers List 2024 is released now. Shakti Dubey is UPSC AIR 1 2024 Topper.
→ Also check Best IAS Coaching in Delhi