Monkeypox, later renamed ‘Mpox’ by WHO, is a rare zoonotic viral disease caused by infection with the Mpox virus. The monkeypox virus belongs to the same family of viruses as the variola virus, the virus that causes smallpox.
Mpox symptoms are similar to smallpox symptoms but milder, and Mpox is rarely fatal. Mpox is not related to chickenpox. ACAM2000, MVA-BN, and JYNNEOS are some of the vaccines available for the Mpox.
Background of Monkeypox
Mpox was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research in Denmark.
- Despite being named “Monkeypox virus,” the source of the disease remains unknown.
- However, African rodents and non-human primates (like monkeys) might harbour the virus and infect people.
- The first human case of Mpox was recorded in a nine-month-old boy in the Democratic Republic of the Congo (DRC) in 1970.
- Before the recent outbreak in 2022, Mpox had been reported in several central and west African countries.
About Monkeypox (MPX) Virus
The Mpox virus has several distinct characteristics based on the structure and specifications of the virus.
Structure
- The Monkeypox (MPX) virus has distinctive surface tubules and a dumbbell-shaped core component.
- It is an enveloped virus with a double‐stranded DNA genome that belongs to the Orthopoxvirus genus of the Poxviridae family.

Variants
- The Mpox virus is categorised into two types i.e., Clade I and Clade II.
- The Clade I type of Mpox virus has a fatality rate of around 10%.
- The infections that caused the recent outbreak of 2022-2023 are from Clade II (or Clade IIb specifically).
- Infections with Clade IIb are rarely fatal.
- More than 99% of people who get this form of the disease are likely to survive.
- However, people with severely weakened immune systems or younger children may get seriously ill or die.
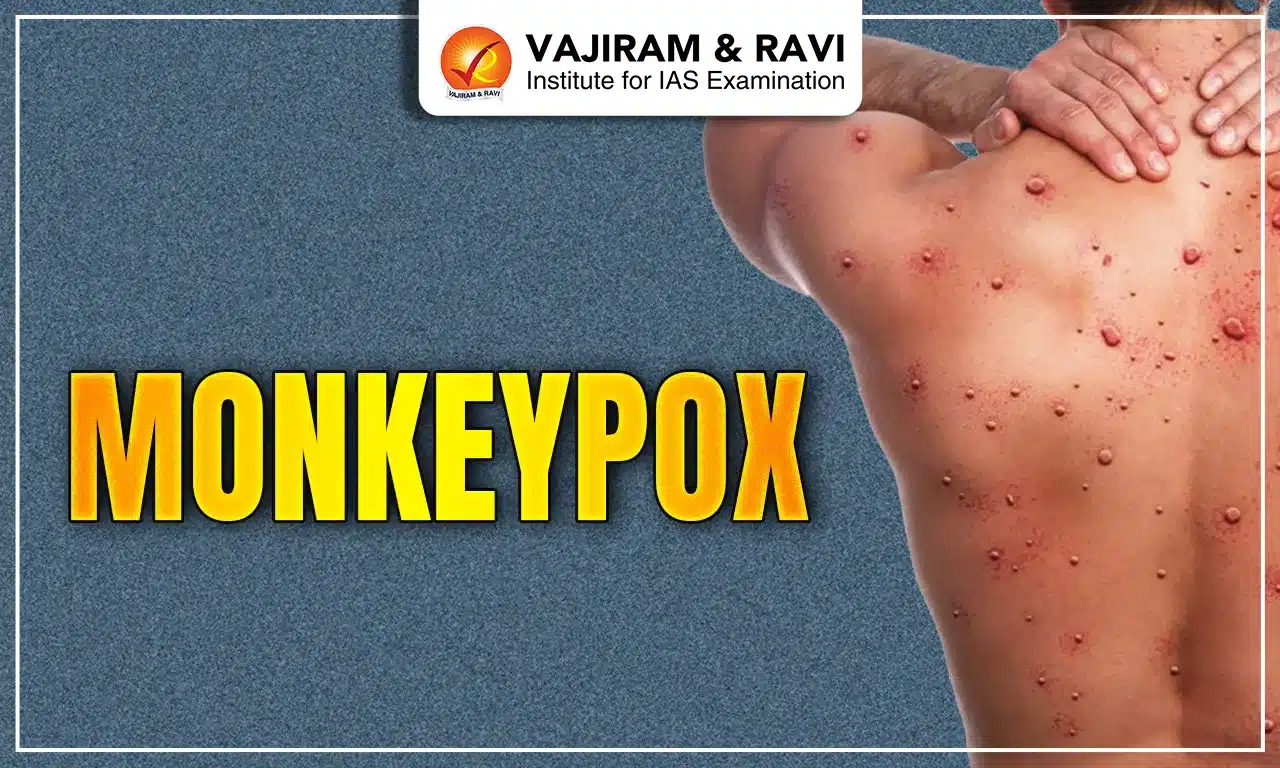
Symptoms of the Monkeypox
The symptoms that people face with Mpox are:
- Rash: It is a major symptom of Mpox as infected persons often get lesions and rashes. It may be located on hands, feet, chest, face, or mouth or near the genitals, including the penis, testicles, labia, vagina, and anus.
- Other Symptoms: There are other symptoms of Mpox that include Fever, Chills, Swollen lymph nodes, fatigue, Muscle aches and backache, Headache, and Respiratory symptoms (for example, sore throat, nasal congestion or cough).
Progression and Transmission of Monkeypox Virus
The disease Mpox is caused by the monkeypox virus (MPXV) which was first seen in monkeys kept for research. Mpox can also be caused due to transmission from person to person or from animal to person. Still, the natural reservoir of this virus is unknown.

Entry and Pathophysiology
- Incubation period: The Mpox virus can enter by multiple routes such as oral, nasal, or skin.
- Then, the virus replicates at these sites and spreads to the local lymph nodes.
- Further, the virus in the blood leads to spread and seeding into other organs.
- This period typically lasts for 7 to 14 days (21 days maximum). During this time, a person does not have symptoms and may feel fine.
- Symptom onset: The secondary viremia leads to 1 to 2 days of prodromal symptoms (period between incubation and the characteristic symptoms) including fever and swelling of lymph nodes first and appearance of lesions later.
- The patients may be contagious now.
- Lesions appear first in the oropharynx followed by its appearance on the skin.
- Serum antibodies are detectable when the lesions appear.
Transmission
- Close or Intimate Contact: Mpox can spread to anyone through close, personal, often skin-to-skin contact, including contact with an infected person as in:
- Mpox rash and scabs from a person with Mpox.
- Saliva, upper respiratory secretions (snot, mucus).
- Areas around the anus, rectum, or vagina.
- Touching Objects: It is less likely but Mpox can get spread by touching surfaces which have not been disinfected.
- By touching objects, fabrics, and surfaces
- Clothing, bedding, towels, fetish gear, sex toys, etc.
- Infected Animals: Some animals can be infected with Mpox and spread it to people through close contact.
- This is more likely with wild animals, specifically small mammals like squirrels, rats, and mice that live in areas where Mpox is endemic (such as in West and Central Africa).
- It is possible that a pet could get infected and spread Mpox to a person during close contact.
- Water In Pools, Hot Tubs: There is no clear link between Mpox and water in pools, hot tubs, or splash pads.
- The Mpox virus is killed in water at the chlorine levels recommended for disinfection in recreational water venues.
- Mpox and Pregnancy: The Mpox virus can be transmitted to the fetus during pregnancy or to the newborn by close contact during and after birth.
Monkeypox Treatment
The goal of treating Mpox is to take care of the rash, manage pain and prevent complications. Early and supportive care is important to help manage symptoms and avoid further problems.
- Isolation: The persons infected by Mpox must be isolated and cared far away from other people.
- Prioritising Vulnerable: It is recommended for people at high-risk health workers, sex workers, etc to get vaccinated to prevent infection with Mpox during an outbreak.
- Medications: Several antivirals, such as tecovirimat, need to be made accessible to the persons infected.
Monkeypox Vaccines
The ACAM2000, MVA-BN, and JYNNEOS vaccines are the available vaccines for controlling the current outbreak.
- The vaccines should be given within 4 days of contact with someone who has Mpox (or within up to 14 days if there are no symptoms).
- MVA-BN: It is a third-generation live, attenuated, nonreplicating, modified vaccinia Ankara vaccine.
- ACAM2000: It is a smallpox vaccine that is also a second-generation live, attenuated vaccinia virus vaccine.
- JYNNEOS vaccine: It is presently being used to treat monkeypox, and was developed using the Modified Vaccinia Ankara (MVA).
- It was employed in the 1970s German smallpox eradication campaign to immunise more than 100,000 people.
- This vaccine is more acceptable as it has limited adverse effects than ACAM2000.
Current Trends of Monkeypox
The World Health Organization had declared monkeypox a Public Health Emergency of International Concern (PHEIC) but later removed this designation in May 2023.
- 2022-2023 Outbreak: The current outbreak of Mpox all over the world is very concerning because:
- There are around 91,328 cases of Mpox across the world.
- In the USA, there were 55 deaths reported out of 31,010 cases of Mpox.
- Cases in India: India reported its first case of monkeypox in July 2022 with the patient having traveled from the UAE to Kerala.
- Till July 2023, a total of 27 confirmed cases of monkeypox were reported in India, with 12 cases from Kerala and 15 from Delhi.
- Most of these cases were characterized as mild, and treatment remained largely supportive.
- Re-infection after vaccination: In June 2023, Israel detected a case of monkeypox in a man who had been vaccinated against the virus but contracted it after travelling from Portugal to Israel.
- Clade 9 Variant: In September 2023, the ICMR National Institute of Virology (ICMR-NIV) identified the presence of the Clade 9 variant of the varicella-zoster virus (VZV) in India for the first time.
India’s Strategy to Deal with Monkeypox
The following are the initiatives taken by India to deal with monkeypox:
- Hospitals Identified: The Ministry of Health and Family Welfare (MOHFW) had proposed guidelines to tackle monkeypox in three significant government hospitals in Delhi.
- Isolation Rooms: The government has also taken steps to make isolation rooms operational in the dedicated hospitals. It was then enlarged to include an additional 10 rooms in three more hospitals.
- Diagnosis: Earlier, the National Institute of Virology (NIV) Pune was the nodal centre for monkeypox diagnosis by RT-PCR test (same used for COVID-19).
- Later, ICMR gave permission to 15 additional institutions to conduct the RT-PCR test for confirmation.
- According to ICMR, all of the recovered monkeypox virus (MPXV) sequences from India are lineages of the A2 which is of clade 2b.
- Vaccines: The Smallpox vaccine was reported to provide approximately 85% protection against human Mpox.
- After the eradication of smallpox from India, vaccination was discontinued in 1980.
Kerala’s Strategy
- The State government has ordered the setting up of screening desks with thermal scanners at all airports and ports for early detection of potential spreaders.
- Hence, suspected cases would be quarantined.
- The health department introduced protocols for hospitals and healthcare personnel like private hospitals would not refer patients with Mpox symptoms to government hospitals.
- Surveillance medical officers have been appointed in all 14 districts.
Way Forward
The best practices followed by countries around the globe can provide a direction to take steps as part of India’s future strategy. The following are a few measures such as:
- Vaccines for the Vulnerable: In the UK, New York City, and Canada, vaccines are currently being provided by prioritising sections of people as per their vulnerability to the virus.
- Training: Providing proper academic training for medical practitioners.
- Targeted Testing: It is necessary to promote health in vulnerable populations with targeted testing and education that is compassionately supported.
- Preventing Stigma: To ensure that public health measures are appropriate and non-stigmatizing and to avoid messaging that will push the outbreak underground.
- Involvement of communities: The communities must be involved from the beginning in structuring the implementation of measures.
- Precautionary Measure: The use of Condoms is encouraged to prevent further spread.
Last updated on November, 2025
→ Check out the latest UPSC Syllabus 2026 here.
→ Join Vajiram & Ravi’s Interview Guidance Programme for expert help to crack your final UPSC stage.
→ UPSC Mains Result 2025 is now out.
→ UPSC Notification 2026 is scheduled to be released on January 14, 2026.
→ UPSC Calendar 2026 is released on 15th May, 2025.
→ The UPSC Vacancy 2025 were released 1129, out of which 979 were for UPSC CSE and remaining 150 are for UPSC IFoS.
→ UPSC Prelims 2026 will be conducted on 24th May, 2026 & UPSC Mains 2026 will be conducted on 21st August 2026.
→ The UPSC Selection Process is of 3 stages-Prelims, Mains and Interview.
→ UPSC Result 2024 is released with latest UPSC Marksheet 2024. Check Now!
→ UPSC Prelims Result 2025 is out now for the CSE held on 25 May 2025.
→ UPSC Toppers List 2024 is released now. Shakti Dubey is UPSC AIR 1 2024 Topper.
→ UPSC Prelims Question Paper 2025 and Unofficial Prelims Answer Key 2025 are available now.
→ UPSC Mains Question Paper 2025 is out for Essay, GS 1, 2, 3 & GS 4.
→ UPSC Mains Indian Language Question Paper 2025 is now out.
→ UPSC Mains Optional Question Paper 2025 is now out.
→ Also check Best IAS Coaching in Delhi
Monkeypox FAQs
Q1. What is the vaccine for Mpox?+
Q2. What is Mpox disease?+
Q3. Is Mpox the same as Monkeypox?+